Number: Mo1411
PREDICTORS OF POST-ERCP PANCREATITIS: A COMPREHENSIVE SYSTEMATIC REVIEW AND META-ANALYSIS OF 229 STUDIES WITH OVER 3.3 MILLION PATIENTS
Society: AGA
Track: Pancreatic Diseases
Introduction: Acute pancreatitis (AP) is the most common complication of endoscopic retrograde cholangiopancreatography (ERCP). A comprehensive understanding of post-ERCP pancreatitis (PEP) risk factors is crucial. Current meta-analyses on PEP risk factors are limited by a small number of studies and the inclusion of data reported as unadjusted risk factors. We aim to assess the predictors of PEP precisely with this rigorous meta-analysis.
Methods: We searched Embase, PubMed, and Web of Science databases for published studies from inception until July 2023. Only studies that used a multivariate model to assess risk factors for PEP were included. Studies reporting unadjusted risk factors were excluded. Pooled adjusted odds ratios (OR) with 95% confidence intervals (CI) for risk factors reported in three studies or more were obtained within a random-effects model.
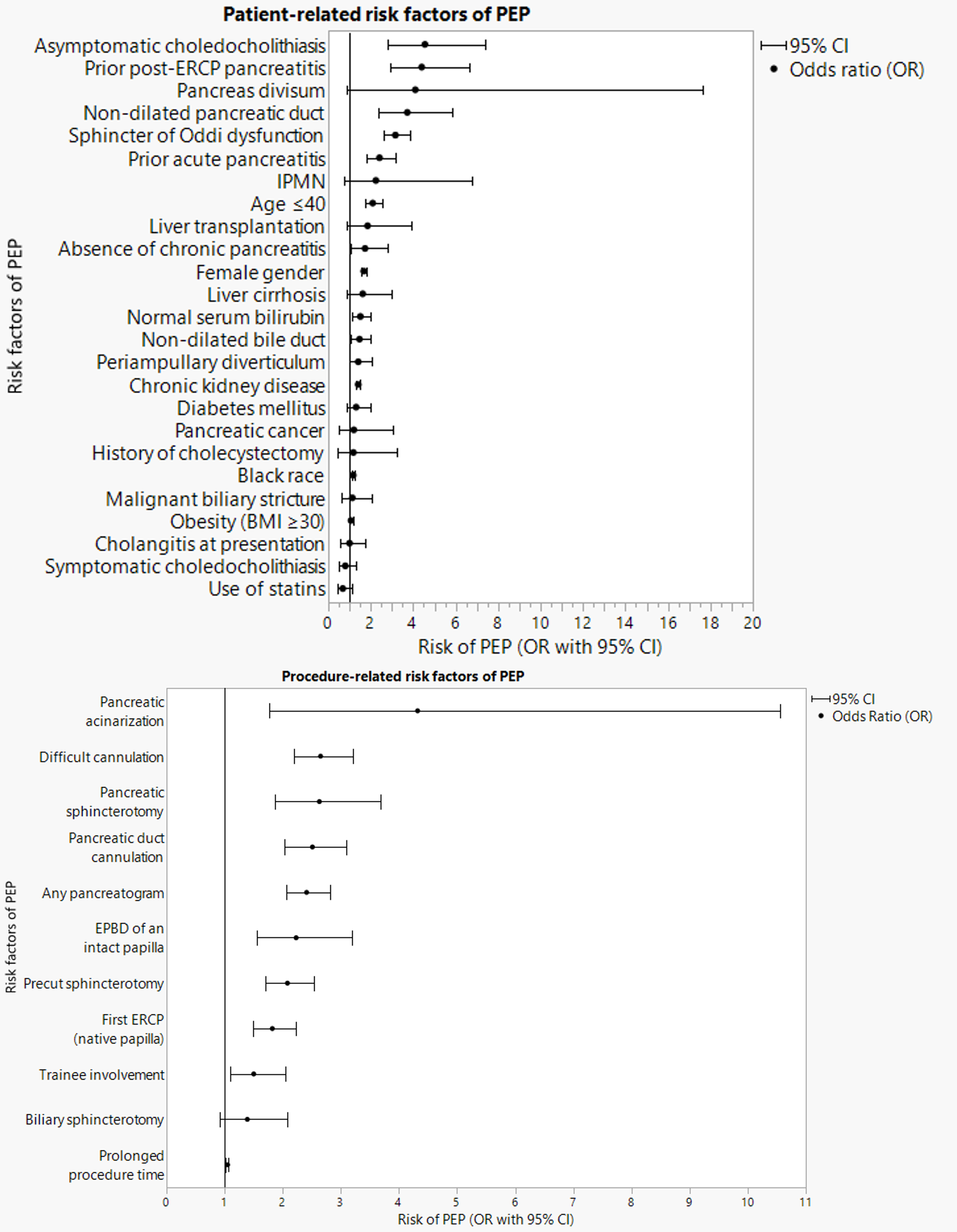
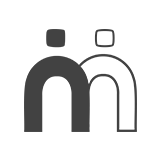
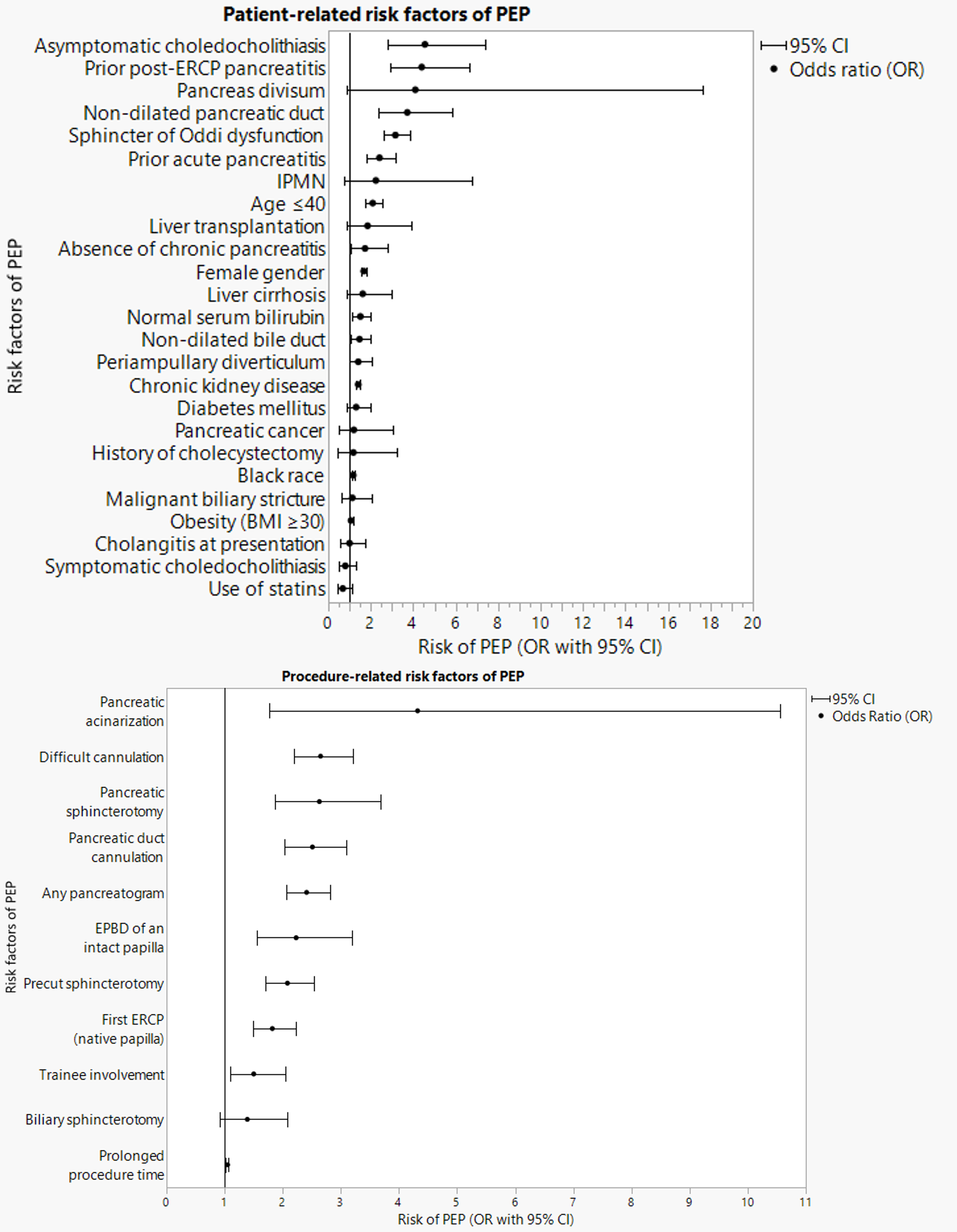
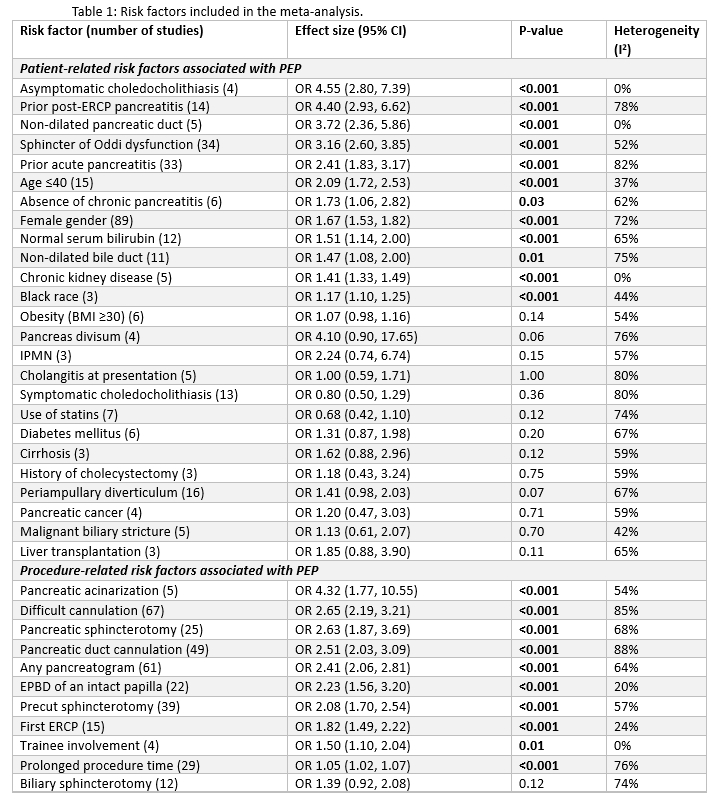
Results: 229 studies with 3,336,491 patients who underwent 3,344,413 ERCPs were included. Thirty-six unique risk factors (25 patient-related and 11 procedure-related) were analyzed (Table 1 & Figure 1). Asymptomatic choledocholithiasis 4.55 (2.80-7.39), prior PEP 4.40 (2.93-6.62), non-dilated pancreatic duct (PD) 3.72 (2.36-5.86), sphincter of Oddi dysfunction 3.16 (2.60-3.85), prior AP 2.41 (1.83-3.17), age ≤40 2.09 (1.72-2.53), absence of chronic pancreatitis 1.73 (1.06-2.82), female gender 1.67 (1.53-1.82), normal serum bilirubin 1.51 (1.14-2.00), non-dilated bile duct 1.47 (1.08-2.00), chronic kidney disease 1.41 (1.33-1.49), and black race 1.17 (1.10-1.25) were significant patient-related predictors of PEP. (Figure 1). Obesity, pancreas divisum, intraductal papillary mucinous neoplasm, cholangitis, symptomatic choledocholithiasis, use of statins, diabetes mellitus, cirrhosis, malignant biliary stricture, pancreatic cancer, periampullary diverticulum, history of cholecystectomy and liver transplant were not associated with increased risk of PEP. Pancreatic acinarization 4.32 (1.77-10.55), difficult cannulation 2.65 (2.19-3.21), pancreatic sphincterotomy 2.63 (1.87-3.69), PD cannulation 2.51 (2.03-3.09), any pancreatogram 2.41 (2.06-2.81), EPBD of an intact papilla 2.23 (1.56-3.20), precut sphincterotomy 2.08 (1.70-2.54), first ERCP (native papilla) 1.82 (1.49-2.22), trainee involvement 1.50 (1.10-2.04) and prolonged procedure time 1.05 (1.02-1.07) were significant procedure-related predictors of PEP. Biliary sphincterotomy was not associated with an increased risk of PEP.
Conclusions: Our meta-analysis focused on adjusted, multivariate risk factors to provide precise estimates of the most important risk factors for PEP. Incorporating our results into a prediction model may reliably identify high-risk patients for PEP, thus aiding physicians in decision-making for ERCP, personalizing the informed consent process for ERCP, and determining the need for more intensive PEP preventive measures.
Number: Mo1411
PREDICTORS OF POST-ERCP PANCREATITIS: A COMPREHENSIVE SYSTEMATIC REVIEW AND META-ANALYSIS OF 229 STUDIES WITH OVER 3.3 MILLION PATIENTS
Society: AGA
Track: Pancreatic Diseases
Introduction: Acute pancreatitis (AP) is the most common complication of endoscopic retrograde cholangiopancreatography (ERCP). A comprehensive understanding of post-ERCP pancreatitis (PEP) risk factors is crucial. Current meta-analyses on PEP risk factors are limited by a small number of studies and the inclusion of data reported as unadjusted risk factors. We aim to assess the predictors of PEP precisely with this rigorous meta-analysis.
Methods: We searched Embase, PubMed, and Web of Science databases for published studies from inception until July 2023. Only studies that used a multivariate model to assess risk factors for PEP were included. Studies reporting unadjusted risk factors were excluded. Pooled adjusted odds ratios (OR) with 95% confidence intervals (CI) for risk factors reported in three studies or more were obtained within a random-effects model.
Results: 229 studies with 3,336,491 patients who underwent 3,344,413 ERCPs were included. Thirty-six unique risk factors (25 patient-related and 11 procedure-related) were analyzed (Table 1 & Figure 1). Asymptomatic choledocholithiasis 4.55 (2.80-7.39), prior PEP 4.40 (2.93-6.62), non-dilated pancreatic duct (PD) 3.72 (2.36-5.86), sphincter of Oddi dysfunction 3.16 (2.60-3.85), prior AP 2.41 (1.83-3.17), age ≤40 2.09 (1.72-2.53), absence of chronic pancreatitis 1.73 (1.06-2.82), female gender 1.67 (1.53-1.82), normal serum bilirubin 1.51 (1.14-2.00), non-dilated bile duct 1.47 (1.08-2.00), chronic kidney disease 1.41 (1.33-1.49), and black race 1.17 (1.10-1.25) were significant patient-related predictors of PEP. (Figure 1). Obesity, pancreas divisum, intraductal papillary mucinous neoplasm, cholangitis, symptomatic choledocholithiasis, use of statins, diabetes mellitus, cirrhosis, malignant biliary stricture, pancreatic cancer, periampullary diverticulum, history of cholecystectomy and liver transplant were not associated with increased risk of PEP. Pancreatic acinarization 4.32 (1.77-10.55), difficult cannulation 2.65 (2.19-3.21), pancreatic sphincterotomy 2.63 (1.87-3.69), PD cannulation 2.51 (2.03-3.09), any pancreatogram 2.41 (2.06-2.81), EPBD of an intact papilla 2.23 (1.56-3.20), precut sphincterotomy 2.08 (1.70-2.54), first ERCP (native papilla) 1.82 (1.49-2.22), trainee involvement 1.50 (1.10-2.04) and prolonged procedure time 1.05 (1.02-1.07) were significant procedure-related predictors of PEP. Biliary sphincterotomy was not associated with an increased risk of PEP.
Conclusions: Our meta-analysis focused on adjusted, multivariate risk factors to provide precise estimates of the most important risk factors for PEP. Incorporating our results into a prediction model may reliably identify high-risk patients for PEP, thus aiding physicians in decision-making for ERCP, personalizing the informed consent process for ERCP, and determining the need for more intensive PEP preventive measures.